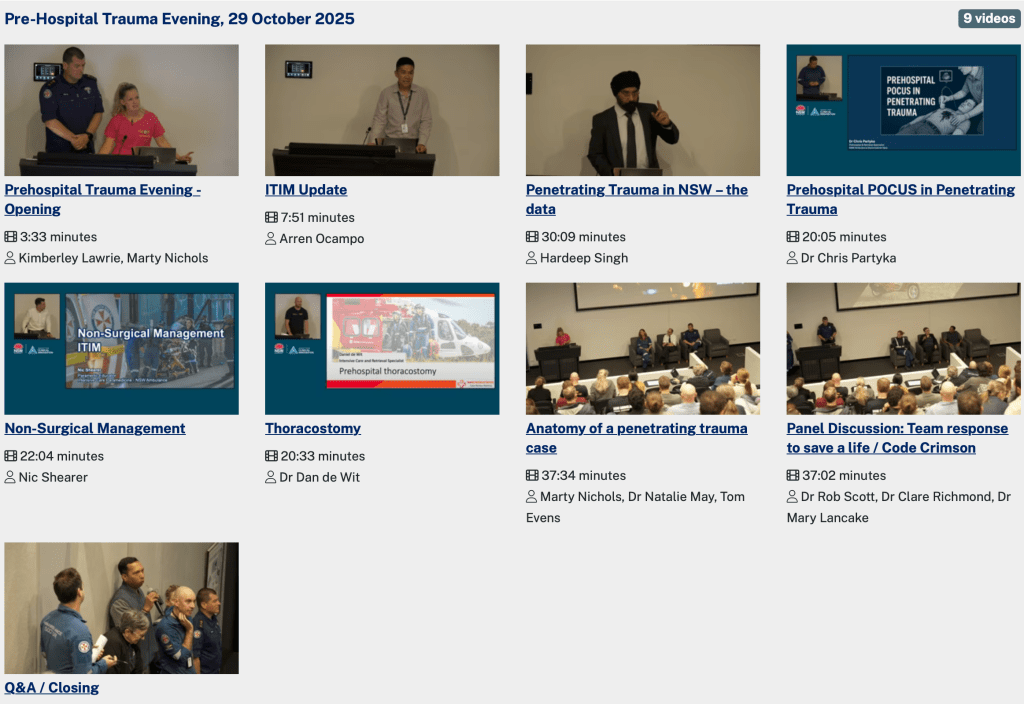
In October 2025, we hosted the ITIM Pre-Hospital Trauma Evening on base, with talks from trauma and prehospital specialists from around the state.
The videos of these talks are available now through the ITIM website – click here to be taken to the video page. You will need to select Pre-Hospital Trauma Evening, 29 October 2025 to see the recorded videos.
Topics include Penetrating Trauma in NSW (Hardeep Singh), Prehospital POCUS in Penetrating Trauma (Chris Partyka), Thoracostomy (Dan De Wit) and Anatomy of a Penetrating Trauma Case (Marty Nichols, Tom Evens and Natalie May).