(Thanks again to Dr. Clare Hayes-Bradley for presenting the latest Airway Registry and penning the subsequent discussion points below.)
To RSI or not to RSI, that is the question…
It’s foul weather, near zero degrees and torrential rain, it’s night, and you’re on a residential street 15 minutes away from the regional trauma centre by road. Your obese patient is unconscious with airway obstruction along with other signs of serious injury. To RSI or not to RSI? What factors might influence your decision making?
In favour of RSI in the vehicle would be the  weather and a lack of nearby shelter (like a car port or service station). In favour of RSI at the hospital might be adequacy of basic airway manoeuvres & ventilation and short travel time. Your assessment of current airway patency and ventilation, together with your assessment of difficulty of intubation and patient positioning inside the vehicle may be factors (like can you physically adjust the stretcher head-up and place occipital padding). There may be other pressing clinical concerns that require urgent hospital intervention.
weather and a lack of nearby shelter (like a car port or service station). In favour of RSI at the hospital might be adequacy of basic airway manoeuvres & ventilation and short travel time. Your assessment of current airway patency and ventilation, together with your assessment of difficulty of intubation and patient positioning inside the vehicle may be factors (like can you physically adjust the stretcher head-up and place occipital padding). There may be other pressing clinical concerns that require urgent hospital intervention.
Our GSA-HEMS PHEA manual 2016 gives some suggestions on the pros and cons for on-scene versus hospital RSI.
Performing an RSI in a vehicle will feel different to an RSI at the back of the road vehicle with 360 degree patient access. Why not practice an ‘in-car’ RSI for your next RSI currency or sim?
My bougie is too rigid…..
Borrowed from prehospitalmed.com, with permission
So you can see the cords but that bougie just won’t go where you want it to – what are your options?
- Consider optimal bougie ‘top control’ by your assistant
- Consider your bougie grip – for example, some practitioners report the ‘Shaka’ or ‘kiwi’ grips can improve bougie tip control
- Take the bougie out of the mouth to re-shape
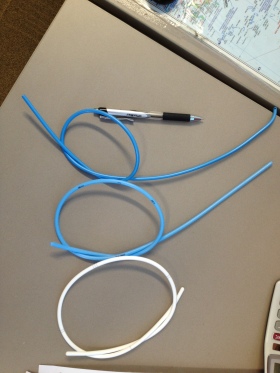
- Use our other bougie (hollow blue or solid white)
- Intubate the trachea without adjuncts if able
- Use a stylet as an alternative adjunct
Another thing to consider practicing at your next RSI currency…
See the PHARM blog for numerous posts on bougie excellence
And from the American College of Emergency Physicians, this bougie article.
Agitation pre-RSI
Patients can appear agitated pre-RSI for many reasons including pain, fear, their pathology/injuries, or drug effects. In some cases IV or IO access for pharmacological control is impossible to achieve initially. Safe physical restraint of the patient to allow intramuscular sedation may be necessary. Needlestick injuries must be in everyone’s mind here and ‘safe sharps’ are paramount. Coordinating the sedation attempt with colleagues with clear language and explanation is important, as is being aware of your location and availability of resuscitation equipment if the response to the sedation is profound.
So what drug or dose would you choose in an adult male patient whom you suspect is agitated from severe pain. Consensus would suggest 2-4mg/kg IM Ketamine could be reasonably expected to produce the desired result – a patient calm enough to accept IV/IO access and further treatment.
Additional Reading
Weingart’s Delayed Sequence Intubation
RFDS document on managing acutely agitated patient in a remote environment

